Nearly 15% of all Americans are currently enrolled in Medicare, with that number expected to double over the next decade. Medicare is a crucial way in which individuals who are at least 65 years of age or have special health conditions get their health care coverage.
As this population grows and more people turn to technology to help them access and enroll in government services, it’s essential that individuals can reliably and easily find and enroll in the Medicare plan that best meets their needs.
In June 2018, the Centers for Medicare & Medicaid Services (CMS) Office of Communication awarded Ad Hoc a contract to modernize the Medicare Plan Finder tool, which allows people to find available plans and enroll. Expanding on the lessons we’ve learned over the years working on HealthCare.gov, we sat down with our partners, Medicare beneficiaries, and those who support and advocate for them to understand deeply the problems and stress people experience when picking coverage. Our goal was to map the future of a tool that would make this process less stressful. Employing the best practices in human-centered design, development, and infrastructure, we worked collaboratively with our government partners to rethink how we could map the experience of the Medicare Plan Finder to meet beneficiary needs.
The goal
Simply put: replace a legacy tool built more than a decade ago with a tool that would make it easier for Medicare beneficiaries, or those who help them, to find and enroll in a Medicare plan that best meets their health and financial needs. To accomplish this, we needed to transform this big vision into a product that could be built to serve people. Though our goal could be written down in one sentence, the path to get there was not so simple. Using Agile development, product thinking, and strategic trade-offs, we worked with our government customers to answer the core questions that would guide our work:
- What does success look like?
- Who is our user?
- What are their pain points?
- How do we prioritize all the features we can build to ensure that we have a strong foundation that we can improve upon in the future?
- How do we ensure that we are continuously gathering feedback from those who will use the tool so we can improve over time?
- How do we ensure that the tool is performant, stable, and reliable?
How we accomplished our goal
Build with the user in mind. Finding and enrolling in Medicare can be a complicated and stressful process, with beneficiaries needing to make important decisions about their health and well-being while trying to navigate a tool with a lot of information. To ensure we built an experience that would guide users while reducing as much stress as we could, we gathered all the information we could get our hands on. This included previous feedback from users, organizations who support them, and reports on the beneficiary pain points. We used this feedback to build a foundation for the new direction we wanted to take the Medicare Plan Finder, while continuing to conduct in-person user testing sessions as we went to validate whether or not we were on the right path.
Build using the best modern development practices while ensuring broad range support for all users. As more individuals turn to technology to access their government services, it’s crucial that we build software that employs the best practices in security, reliability, and performance. We also must reduce complexity to ensure that anyone, no matter where they live, the quality of their internet access, or the version of their device has the same ability to use the site. Being stewards for how individuals find and enroll in Medicare means that we must think critically about how we build our tools to ensure that the information of the millions of beneficiaries who come to Medicare Plan Finder is secure and safe. We used these principles of longevity and security to ensure that the Medicare Plan Finder would be available and accessible to everyone.
Determine the cost of drugs under a Medicare plan and pharmacy. For many beneficiaries, the cost of their various prescription drugs is their biggest concern, directly impacting their financial state and thus the plan in which they ultimately enroll. It was important for us to try to give beneficiaries the best cost estimate for their drugs with a given plan and pharmacy so that they could make a plan choice that best met their health and financial needs. This required us to distill down disparate pieces of policy in order to build an algorithm that would account for the various Medicare coverage phases and how drugs are covered by different plans. By doing so, we can go beyond telling beneficiaries if a drug is covered to estimating how they will collectively pay for all of their drugs over the course of the year.
What we built
The redesigned Medicare Plan Finder focuses on personalizing the Medicare plan shopping experience for beneficiaries and those who help them. This is what we built to accomplish this:
Three key user experiences
Medicare Plan Finder provides three distinct user experiences to ease the experience of beneficiaries and those who support them.
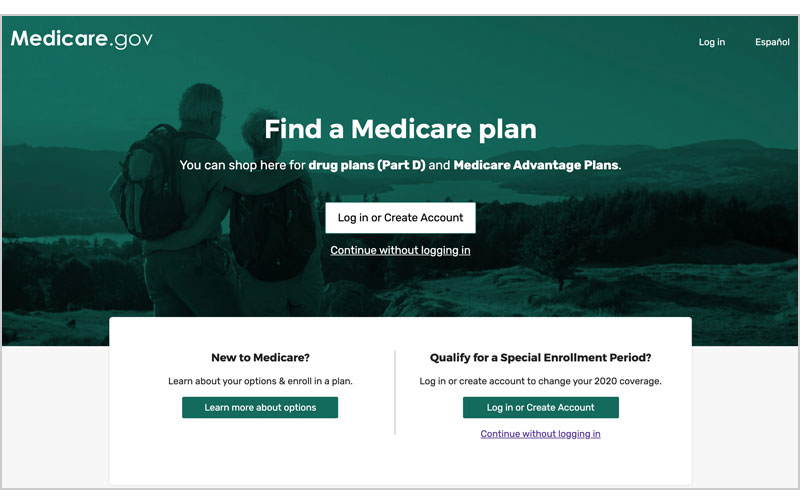
- The anonymous experience. Given the comfort of the Medicare beneficiary population with technology and sharing their information, it was crucial to provide a way for beneficiaries to view plans without providing any personal information. This allows anyone to quickly go into the tool, answer a few key questions, input their drugs and pharmacies if prefered, then view plans. Users are then presented with key pieces of information crucial to the decision making process and are able to filter and sort plans to best meet their needs. From there, they can choose to compare a number of plans or view one plan’s details to better evaluate how comprehensive the plan is relative to their needs. Once an individual has found a plan they prefer, they enroll by submitting an application that will then be forwarded to insurance companies to process.
- The logged in experience. Building on the anonymous experience, beneficiaries are able to create a Medicare.gov account to get a more personalized experience. Through this logged-in experience, Medicare Plan Finder is able to provide beneficiaries with key pieces of information about themselves to streamline the plan selection and enrollment process, including prescription drugs they’ve previously taken and their current coverage. We’re also able to pre-fill parts of the enrollment application to save everyone time.
- The customer service representative experience. Sometimes you need a little help and would like to talk to someone on the phone. When calling 1-800-Medicare, you’re paired with a customer service representative who can guide you through the experience. This additional user experience allows customer service representatives to effectively log-in as a beneficiary and help pull up information about the beneficiary to help them find a plan that best meets their needs.
A drug search experience and pricing engine
As mentioned before, how much a beneficiary will have to pay for their drugs over the course of the year greatly impacts their financial, physical, and emotional well-being. From our user research, it quickly became clear that drug costs are one of the most stressful and most important decision points for a beneficiary. But, Medicare drug pricing is quite complicated, all impacted by a complex mix of policy, how a plan and pharmacy covers a drug, what tier that drug is on, and how the drug moves through the Medicare coverage phases. Rather than overwhelm users with all that complexity, we worked to understand what level of information was most useful to beneficiaries when thinking about their drug costs. From these user testing interviews and research sessions, we discovered that there were three key pieces of information beneficiaries wanted to know when it came to which plan best covers their health needs:
- The cost of an individual drug across the Medicare coverage phases.
- The cost of your set of drugs across the Medicare coverage phases for each month, and therefore, what you would expect to pay in January vs August.
- The total estimated cost for a set of drugs with a pharmacy under a specific plan for the year.
With this understanding, we worked closely with our government partners to ensure that our drug pricing calculations matched the various drug policies written by CMS, allowing us to account for complexities and nuances when providing drug estimates. We’ve also worked to ensure that our estimates remain up to date with any changes that plans make to how they cover certain drugs and certain pharmacies.
By being able to calculate and display these drug pricing data points to our users, we’re able to give people crucial information that will help them decide which plan best meets their health and financial needs. Because policies and how drugs get covered evolve and change over time, we work with our government partners to ensure that our calculations continue to evolve to match the latest circumstances.


What we’ve accomplished so far
Since CMS launched the redesigned Medicare Plan Finder, the tool has:
- Helped more than 2.6 million Medicare beneficiaries enroll in a Medicare plan, about 40% more enrollments than the legacy tool the previous year
- During Medicare’s Open Enrollment, the redesigned Medicare Plan Finder saw an average of 373,000 visitors a day and peaked at 847 API requests per second.
- Zero downtime for the redesigned Medicare Plan Finder, meaning the tool ran smoothly and did not impact an individual’s ability to find and enroll in Medicare
But most importantly, here are some quotes from the beneficiaries who used the redesigned Medicare Plan Finder:
“I really like it because it’s self-explanatory and gives things in detail. You know up front what each plan costs a month, what your deductibles are, and what drugs are covered and what drugs aren’t. That’s really important. It gives you an estimate right up front.”
“Even I, a 73-year-old guy who’s not very computer savvy can figure it out.”
“They care enough to construct something like this.”
What’s next
Working on the redesigned Medicare Plan Finder for the last year and a half has been an amazing opportunity to learn more about ways in which Ad Hoc can support CMS and Medicare beneficiaries. We’ve been able to go into the depths of the Medicare world and the pain points beneficiaries feel with our partners at CMS, working strategically and collaboratively to chart a path forward for how we can continue to evolve the Medicare Plan Finder with the needs of beneficiaries.
Our approach to the Medicare Plan Finder was to build a tool and process that would allow us to continuously improve what we provided to beneficiaries and those who support them. As we move forward in our work with CMS, we’ll continue to gather feedback from users, stakeholders, advocacy groups, and other external voices to understand new pain points that arise or areas that we can improve. It’s crucial to us that our tools evolve alongside the ways in which user needs evolve so that we continue to provide clarity and ease to an important process.


